Hampshire and Isle of Wight Integrated Care System has a long history of working together with local partners to enable people in our communities to live healthier, longer lives. By working in partnership, we can provide more consistency of care, break down barriers between services and reduce health inequalities.
What are health inequalities?
Health inequalities are about differences in the status of people’s health. But the term is also used to refer to differences in the care that people receive and the opportunities that they have to lead healthy lives – both of which can contribute to their health status.
Health inequalities can therefore involve differences in:
- health status, for example, life expectancy
- access to care, for example, availability of given services
- quality and experience of care, for example, levels of patient satisfaction
- behavioural risks to health, for example, smoking rates
- wider determinants of health, for example, quality of housing
Addressing these inequalities is a priority that runs throughout our Integrated Care System strategy. Our aim is to provide care that is tailored to individual needs, delivered at the right time and in the right place.
We are delivering on a number of projects to tackle health inequalities across Hampshire and Isle of Wight, which helps us to achieve the four overarching aims of all Integrated Care Systems set by NHS England. These are:
- improve outcomes in population health and healthcare
- tackle inequalities in outcomes, experience and access
- enhance productivity and value for money
- help the NHS support broader social and economic development
By transforming how we engage and support people living with multiple disadvantages, we can include and treat people equally and fairly in a more person-led way.
Health inequalities and equality legal duties
This NHS England Guidance explains the legal rules that NHS organisations including local integrated care boards like Hampshire and Isle of Wight ICB must follow to tackle unfair health gaps and support equality. It says the NHS has a duty to reduce differences in people’s access to care and the outcomes they experience. At the same time, it’s bound by the Equality Act 2010 to prevent discrimination, promote fairness between groups (such as ethnicity, disability, age, etc.), and foster good relations. These two sets of duties reducing health inequalities and upholding equality are separate but connected. NHS bodies must embed both in how they plan, deliver, and evaluate services not just as a legal “tick box,” but as a core part of improving care for everyone.
What do health inequalities look like in...
People in the most deprived parts of Hampshire and the Isle of Wight live shorter and less healthy lives. In some areas, men live up to 6-7 years less than those in affluent areas and spend more years in poor health. Places like Gosport, Havant, and Rushmoor have higher child poverty, more early deaths, and worse long-term conditions.
Joint Strategic Needs Assessment (JSNA) - Hampshire County Council
The Isle of Wight has an ageing population, with nearly 30% aged 65+, much higher than the national average. While many report good health, 5.8% say their health is bad or very bad. Deprivation is high in some areas like Ryde and Freshwater, leading to health issues such as early deaths, long-term illness, and higher rates of self-harm and alcohol-related harm.
Portsmouth faces clear health inequalities linked to poverty and low income. Many children live in low income households, and people in deprived areas have shorter life expectancies. People on low incomes earn less and often struggle with the rising cost of living, leading to more use of food banks and fuel poverty. These challenges affect health and well-being, showing a need for focused support to help those most in need.
Joint Strategic Needs Assessment (JSNA) - Portsmouth City Council
In Southampton, health is worse than the national average, with people living fewer healthy years about 59 years for both men and women. Over two-thirds of adults are overweight or obese, and nearly 10% of pregnant women smoke. These problems show clear health inequalities linked to social and economic issues, needing focused action to improve.
Our approach
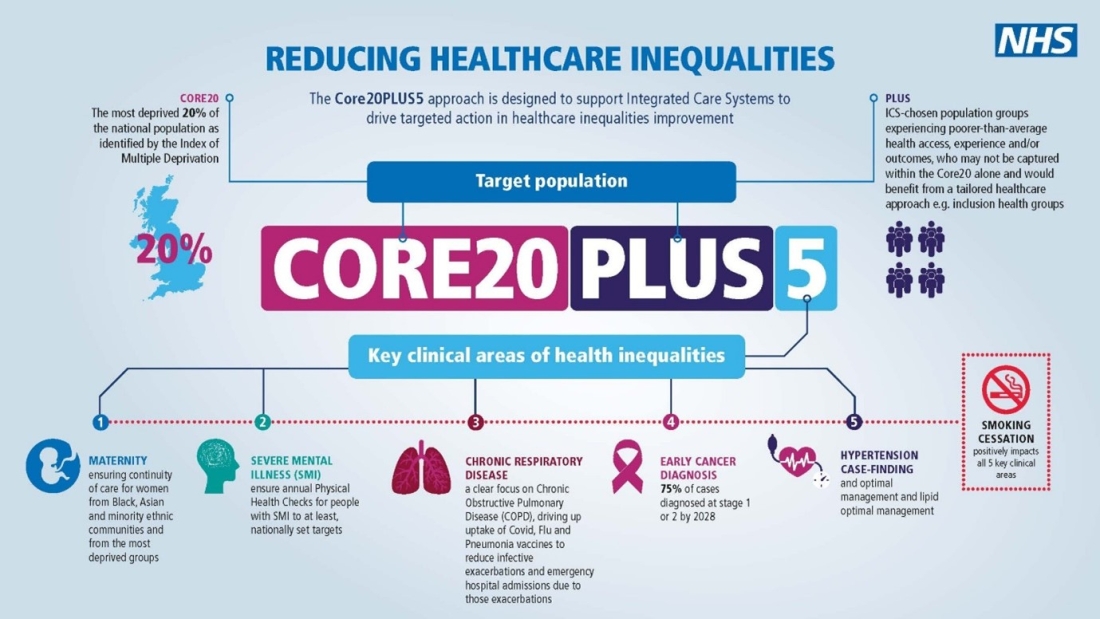
Core20PLUS5 is a framework designed to support the NHS in taking action to address healthcare inequalities.
It covers both adults and children, physical and mental health, and primary and secondary prevention.
It focuses on health disparities i.e. the difference in health outcomes and access to healthcare services that are observable between different populations. By starting with 20% most deprived, using the Index of Multiple Deprivation (IMD), it considers wider inequalities, since IMD is constructed from multiple indicators including areas like unemployment, education, barriers to housing etc.
Core 20
The way this is defined in Core20PLUS5 is 20% most deprived nationally. So, it takes a view of Hampshire and Isle of Wight in the context of the rest of England.
PLUS
PLUS populations recognise that if you just look at national data and IMD, you will miss important populations and communities. This gives ICBs an opportunity to look at their own local data and identify any local communities that are important in their areas.
The Hampshire and Isle of Wight ICP Prevention and Inequalities Board, led by our Public Health teams, worked with NHS Hampshire and Isle of Wight to consider our local data and identify our adult and children and young people PLUS populations. These are groups that we have agreed to work on together at scale. Its important to note that there may be other ‘Plus’ priority population in each of our places that you may wish to prioritise e.g. Veterans in Gosport Borough.
5 - Clinical areas
Adults
The five clinical areas contribute most to the gap in life expectancy between the most and least deprived by broad cause of death. The actions within them identify specific actions the whole NHS can do in relation to primary and secondary prevention.
If you look at the drivers of growth in demand for healthcare Services over the next 15 years, the Core20plus5 clinical areas pick up five of the top 10 drivers, including the top two – Heart Failure will grow by 92% and Atrial Fibrillation by 51% by 2040.
Smoking sits across the top as it is biggest primary prevention area that contributes to the five clinical areas, and is the most effective, evidence base intervention, that contributes most to the gap in life expectancy.
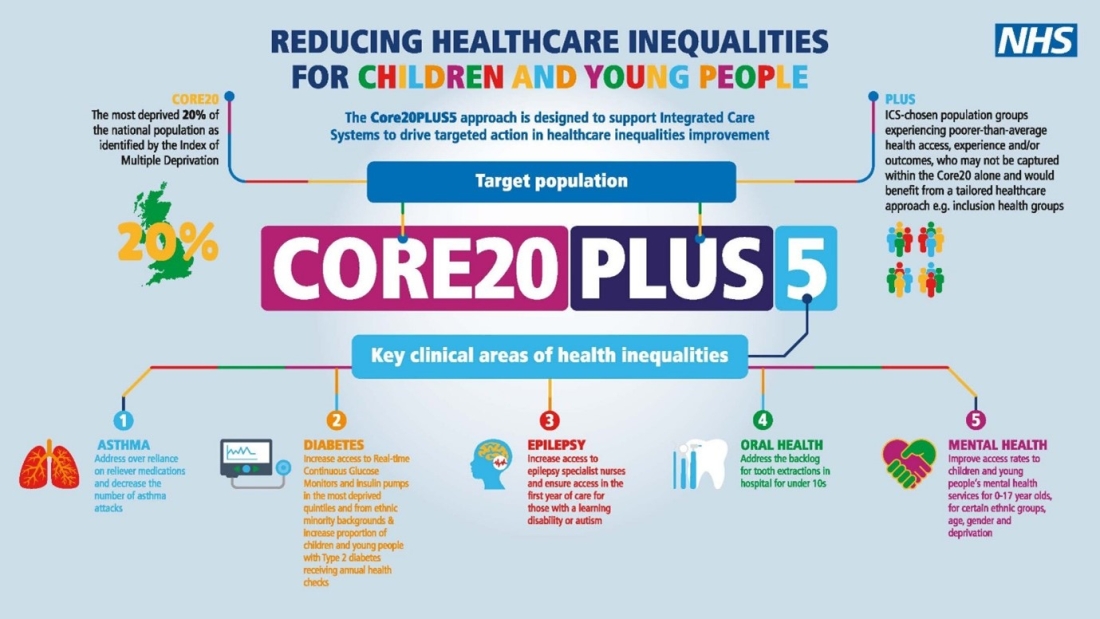
Children and Young People
The NEL admission rates are higher amongst those in the least deprived in the five clinical areas.
For every decile that you drop down in terms of deprivation, child mortality increases by 10%. They include areas that are totally within the gift of the NHS to change. They also include both physical and mental health.
5 Clinical Areas - Adults
- Hypertension case-finding and optimal management and lipid optimal management - To allow for interventions to optimise blood pressure and minimise the risk of myocardial infarction and stroke.
- Early cancer diagnosis - 75% of cases diagnosed at stage 1 or 2 by 2028.
- Chronic respiratory disease - A clear focus on Chronic Obstructive Pulmonary Disease (COPD) driving up uptake of COVID, flu and pneumonia vaccines to reduce infective exacerbations and emergency hospital admissions due to those exacerbations.
- Severe Mental Illness (SMI) - Ensure annual physical health checks for people with SMI to at least nationally set targets.
- Maternity - Ensuring continuity of care for women from Black, Asian and minority ethnic communities and from the most deprived groups. This model of care requires appropriate staffing levels to be implemented safely.
Smoking
- Maternity - One in 10 women smoked at the time of delivery in 2019/20.
- Mental Health - Mental Health conditions are associated with higher rates of smoking and are particularly high amongst those with Serious Mental Illness.
- Chronic respiratory disease - Stopping smoking leads to immediate improvements in respiratory health.
- Early cancer diagnosis - Smoking is a major cause or preventative cancer and common case of those often detected late such as lung and bowel cancer.
- Hypertension - About 70% of CVD cases are attributable to modifiable risk factors with smoking the leading behaviour factor.
5 Clinical Areas - Children & Young People
- Asthma - Address over reliance on reliever medications and decrease the number of asthma attacks.
- Diabetes - Increase access to real-time continuous glucose monitors and insulin pumps across the most deprived quintiles and from ethnic minority backgrounds. And increase proportion of those with Type 2 diabetes receiving recommended NICE care processes.
- Epilepsy - Increase access to epilepsy specialist nurses and ensure access in the first year of care for those with a learning disability or autism.
- Oral health - Tooth extractions due to decay for children admitted as inpatients in hospital, aged 10 years and under.
- Mental health - Improve access rates to children and young people’s mental health services for 0-17 year olds, for certain ethnic groups, age, gender and deprivation.
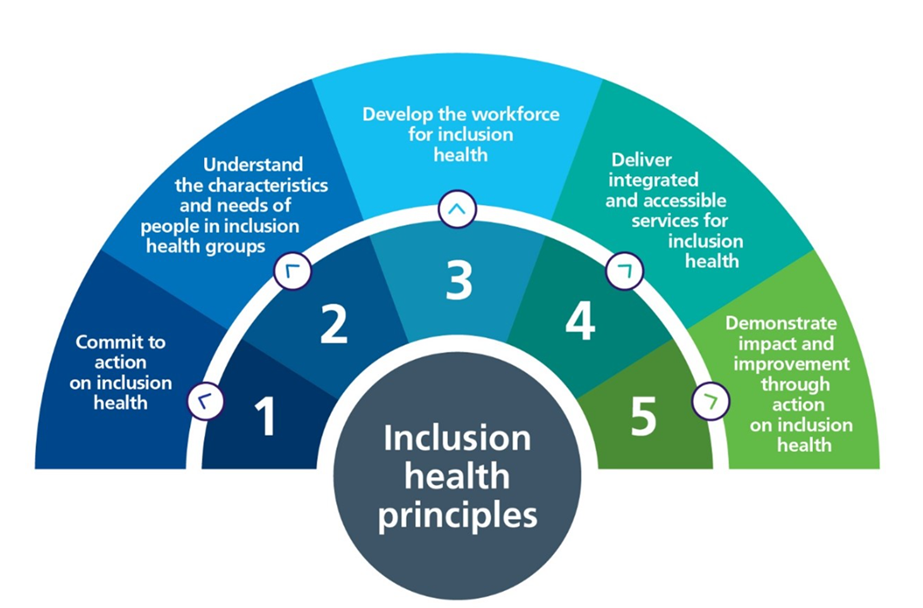
Hampshire & Isle of Wight ICB is following the NHS’s National Framework for Action on Inclusion Health, to reduce health inequalities affecting socially excluded communities such as people experiencing homelessness, substance misuse, Gypsy, Roma, and Traveller communities, sex workers, vulnerable migrant communities and other marginalised groups.
The ICB is committed to five guiding principles: (1) commit to action; (2) understand local lived experience and needs; (3) develop a workforce trained in trauma informed, inclusive care; (4) deliver integrated, accessible services with VCSE partners; and (5) track.
Working closely with voluntary and community organisations and with people with lived experience the system is shaping services that are welcoming, co designed, data informed and compassionate. Through partnerships with housing, public health, social care and local authorities, the ICB is embedding joined up response to social determinants, offering outreach, peer support, flexible access points and personalised care pathways. It actively evaluates impact to ensure improvements in access, quality and outcomes for those most marginalised, in line with its legal duties under the Public Sector Equality Duty and Core20PLUS5 priorities and demonstrate meaningful improvement.
What are we doing to tackle health inequalities?
We are taking targeted action to reduce health inequalities across our communities. This includes delivering dedicated programmes to help people stop smoking, supporting individuals with alcohol dependency, and providing care for those living with diabetes, heart conditions, and mental health challenges.
To build capacity within our workforce, we have trained over 30 Core20PLUS5 Ambassadors and established a Population Health Academy to equip NHS staff with the skills to deliver fairer, more inclusive care.
We have improved data access for local GPs and hospitals, enabling them to identify care gaps and target improvements more effectively.
Working alongside key stakeholders, we actively engage with inclusion health groups, including ethnic minority communities, people experiencing homelessness, and Gypsy, Roma, and Traveller communities, to ensure services meet their needs.
Through collaboration with providers, we have supported the delivery of in-reach clinics offering COVID-19 and flu vaccinations, community blood pressure monitoring, health information events, and mobile dental services, all aimed at reaching the most vulnerable members of our population.