Winner of the PrescQipp 2025 award for Patient Safety and addressing over prescribing

Winner - Hampshire PCN C.difficile improvement project (2025)
In response to a post-pandemic rise in Clostridioides Difficile Infections (CDI) cases, the NHS Hampshire and Isle of Wight Infection Prevention and Control (IPC) team were successful in a bid for Hampshire County Council funding for a targeted intervention using the Contain Outbreak Management Fund (COMF).
This innovative project aimed to reduce CDI incidence and improve patient outcomes by empowering Primary Care Networks (PCNs) with education, data insights, and locally driven quality improvement (QI) initiatives. The project was also aimed at all interested staff groups, offering the opportunity for those aiming to improve their QI skills; there was a broad mix of project leads from Practice Managers, Nurses, Pharmacists, GP trainees’ and GP’s.
The project launched in September 2024 with a training session for PCN leads, focusing on CDI pathophysiology, prevention, and project expectations. Participating PCNs—selected based on high CDI case rates and populations with increased health inequalities—reviewed at least five local CDI cases each, analysing patient demographics, medical history, antibiotic use, treatment timelines, and coding accuracy.
Insights from these reviews informed local QI projects, implemented by December 2024. These included initiatives such as proton pump inhibitor (PPI) de-prescribing protocols, improved antibiotic stewardship, timely stool sampling, and accurate patient coding. Each intervention addressed specific local themes, ensuring relevance and sustainability. By March 2025, PCNs had completed repeat audits to assess impact and identify further actions.
This webpage has been created to house all of the educational materials, case review data, and project plans into a resource pack to allow practice or PCN to undertake their own local project and to use the project resources.
Outcomes so far:
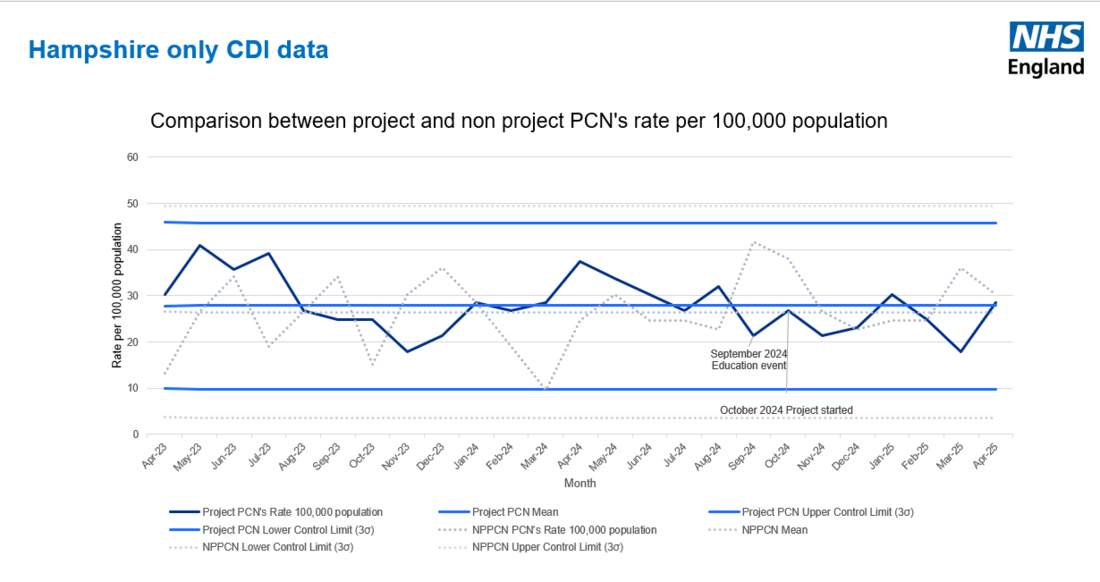
While full 12-month data is pending, early indicators at 8 months suggest reduced CDI cases in the improved awareness, prescribing and CDI management practices in participating PCNs.

 Each PCN implemented at least one QI initiative, with early audits indicating improvements in:
Each PCN implemented at least one QI initiative, with early audits indicating improvements in:
- CDI numbers, with an average predicted reduction in CDI cases of 20% in the project group; this equates to 40 less CDI cases in the 12 month period
- Timely stool sampling; one PCN increased their testing from 25 to 99; while their CDI numbers didn’t decrease, the speed of diagnosis improved which will have had a positive impact on patient safety
- Reduction in unnecessary PPI prescribing: PCN’s successfully deprescribed a number of patients, one PCN contacted 67 patients, with 48% responding; 7 patients chose not to change their PPI prescription, 11 patients arranged a telephone consultation and 14 patients stopped without a consultation and followed the guidance letter.
- Improved antibiotic stewardship
- More accurate patient coding and alerts
- Staff and patient knowledge; one PCN undertook pre and post staff surveys. Their surveys demonstrated improved knowledge and confidence amongst staff with awareness of complications increasing from 42.9% of staff to greater than 95% of staff. 85.7% of the clinicians in the PCN reported that the training and educational materials have had a positive impact on their clinical practice.
Beyond numerical outcomes, the project should have a significant qualitative impact and legacy:
• Increased awareness of CDI among primary care staff
• Enhanced clinical decision-making through education and case-based learning
• Empowerment of frontline teams to lead sustainable change
Next steps:
- Share the learning with practices across Hampshire and Isle of Wight
- Create intervention briefs for each of the four main project groups
- Support practices who wish to undertake their own case reviews
- Add C.difficile data by practice and PCN to the Medicine Optimisation Teams dashboard to allow practices to compare their rates against similar practices
- Collaborate with local colleagues to create an staff education video and clinical meeting discussion prompts
Project resources:
This section contains a suite of resources developed by NHS Hampshire and Isle of Wight Integrated Care Board (ICB) to support Primary Care Networks (PCNs) in designing and delivering their own Quality Improvement (QI) projects. These materials were created to provide structure, guidance, and practical tools for PCN teams, enabling them to identify local priorities, implement change, and measure impact effectively.
The approach taken by the ICB was to facilitate and empower PCNs to lead their own projects, while offering consistent support and shared learning opportunities. Topics ranged from prescribing safety and coding accuracy to patient engagement and long-term condition management.
These resources are shared here to support other ICBs or organisations interested in adopting a similar model. They can be adapted to suit local needs and used to encourage collaborative improvement across multiple PCNs.
- Project plan - please note that due to high demand extra funding was identified for a total of 15 PCN's; this was partially achieved by moving the celebration event to online rather than in person
- PCN project information
- Expression of interest - presentation 1
- Expression of interest - presentation 2
- Education session
- CDI case review template
- C.difficile information page on ICB web page
The following are links to the MS teams forms used to keep track of the project - these links will allow you to duplicate and edit the form for your own use:
Welcome to the PPI resource section for our Primary Care Quality Improvement Projects. This space brings together a range of tools, guidance documents, and support materials designed by PCN teams to deliver impactful change in clinical practice.
One of the most widely explored topics across the projects was PPI deprescribing; a key area in improving medicines safety and reducing unnecessary long-term prescribing. To support this work, teams were provided with a tailored PPI deprescribing resource developed by a member of the Medicines Optimisation Team at NHS Hampshire and Isle of Wight ICB. This resource offers practical advice, evidence-based recommendations, and patient communication tools to guide safe and effective deprescribing in primary care settings.
Explore the materials below to support your ongoing work and share learning across teams.
NHS Hampshire and IOW ICB PPI deprescribing resource:
- Proton pump inhibitors (PPI)
- Hampshire and IOW ICB Medicine Optimisation Team have developed a resource to support the safe deprescribing of PPI's: Reducing inappropriate prescriptions for Proton Pump Inhibitors (PPIs) for risk reduction of Clostridioides difficile infections (CDI).
Accurx messages:
Patient letters and leaflets:
- Lifestyle management (Swan)
- Reducing your PPI patient letter (Winchester Rural North and East)
- Should I keep taking my acid reflux medication deprescribing.org?
Deprescribing guides:
- PPI and CDI prevention step by step guide
- Practice policy
- Prescriber information pack
- PPI deprescribing algorithm deprescribing.org
Other resources:
- Share point resource example
- Winchester Rural North and East Presentation
- CDI project presentation (Swan)
- PPI related project - summarys
Several Primary Care Networks (PCNs) have chosen to centre their projects around education—targeting both healthcare staff and patients. These initiatives have clearly demonstrated the value of raising awareness among clinical teams while also empowering patients to better understand their personal risk factors for infection.
By investing in education, PCNs are not only enhancing clinical knowledge and infection control practices but also fostering a culture where patients feel informed and confident in managing their own health. This dual approach strengthens prevention efforts and supports safer, more proactive care across communities.
Explore the resources below to learn more about these impactful projects and access tools to support education in your own setting:
Accurate clinical coding plays a vital role in ensuring high-quality patient care, effective population health management, and appropriate service planning. This section brings together resources developed by Primary Care Network (PCN) teams aimed at improving coding practices and enhancing staff awareness of key patient risk factors.
These materials have been designed to help teams code patients appropriately, ensuring that important clinical information is captured reliably and consistently. By improving coding accuracy, practices can better identify patients at risk, support proactive care planning, and contribute to more meaningful data for local and national reporting.
Explore the tools, guides, and training materials below to support your team in embedding good coding habits and improving patient outcomes.
Safe, effective, and evidence-based prescribing is central to high-quality patient care. This section provides a collection of resources developed to support Primary Care Network (PCN) teams in enhancing prescribing practices across a range of clinical areas.
These materials aim to help clinicians make informed prescribing decisions, reduce medicines-related harm, and promote cost-effective use of NHS resources. Whether you're reviewing repeat prescriptions, tackling polypharmacy, or implementing deprescribing initiatives, the tools and guidance here are designed to support your team in delivering safer and more personalised care.
Explore the resources and information below to strengthen prescribing processes and improve outcomes for your patients.
PCN project materials:
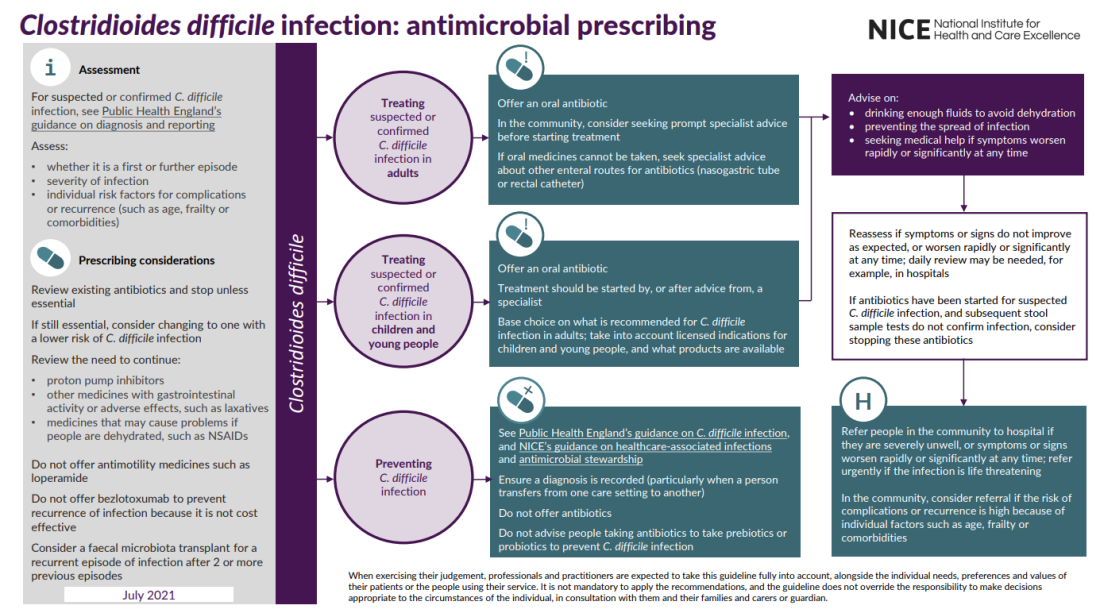
Prescribing considerations for patients who have tested positive or who are considered at high risk of developing C.difficile, please review existing:
- Antibiotics and stop unless essential If still essential, consider changing to one with a lower risk of C. difficile infection Review the need to continue.
- Proton pump inhibitors (PPI)
- Hampshire and IOW ICB Medicine Optimisation Team have developed a resource to support the safe deprescribing of PPI's: Reducing inappropriate prescriptions for Proton Pump Inhibitors (PPIs) for risk reduction of Clostridioides difficile infections (CDI).
- Other medicines with gastrointestinal activity or adverse effects, such as laxatives
- Medicines that may cause problems if people are dehydrated, such as NSAIDs.
- Do not offer antimotility medicines such as loperamide.
- Do not offer Bezlotoxumab to prevent recurrence of infection because it is not cost effective. Bezlotoxumab | Drugs | BNF | NICE
- Consider a faecal microbiota transplant FMT for a recurrent episode of infection after 2 or more previous episodes
- For more information on Faecal microbiota transplant (FMT) please see the University of Birmingham Microbiome Treatment Centre web page
- If you are a clinician and wish to discuss FMT for a specific patient please contact your local trusts microbiolgy team via the trusts switchboard
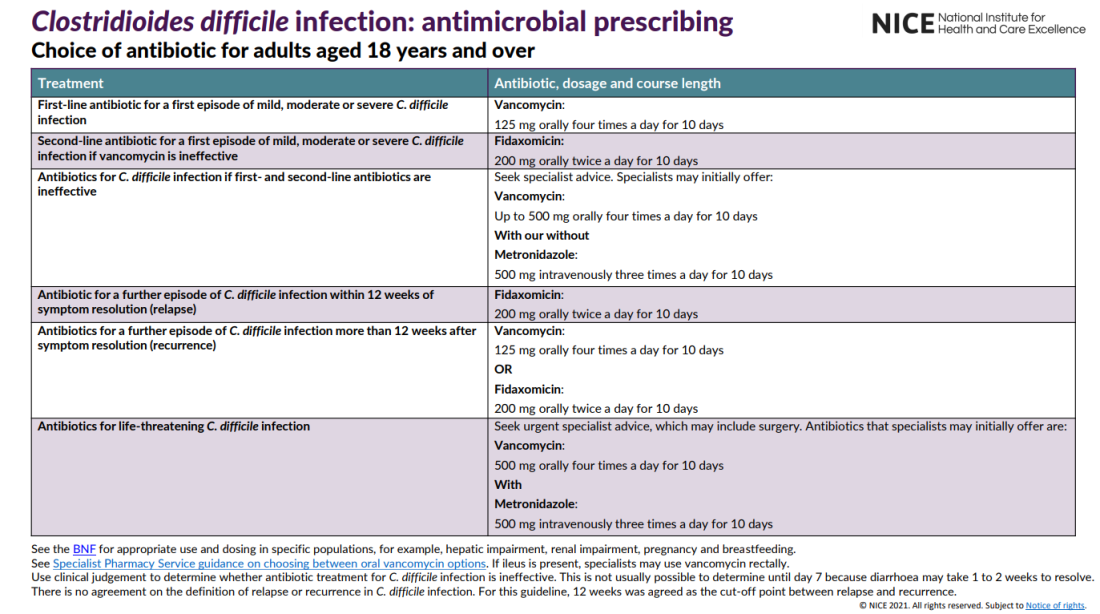
Overview | Clostridioides difficile infection: antimicrobial prescribing | Guidance | NICENG199 visual summary (nice.org.uk)