The government has an ambition for England to become smokefree by 2030, defined as adult smoking prevalence of 5% or less.
Stopping the start: our new plan to create a smokefree generation - GOV.UK
To achieve the government’s targets, The NHS Long Term Plan (LTP) sets out the following ambitions for NHS funded tobacco dependency treatment:
- By 2023/24, all people admitted to hospital who smoke will be offered NHS-funded tobacco treatment services.
- The model will also be adapted for expectant mothers, and their partners, with a new smoke-free pregnancy pathway including focused sessions and treatments.
- A new universal smoking cessation offer will also be available as part of specialist mental health services for long-term users of specialist mental health, and in learning disability services.
The recommended model is based on delivering systematic in-house treatment of tobacco dependence in secondary care. Patients are provided with behavioural support, nicotine replacement therapy (NRT) or other pharmacotherapy during their hospitalisation, with follow up post-discharge. This model was based on the Greater Manchester CURE Project (inpatients) and the Ottawa Model.
Across Hampshire and Isle of Wight patient pathways have been implemented in acute, maternity and inpatient mental health settings, in accordance with the directives of the NHS LTP and the ambitions to achieve Smokefree 2030.
The patient pathway models are detailed here:
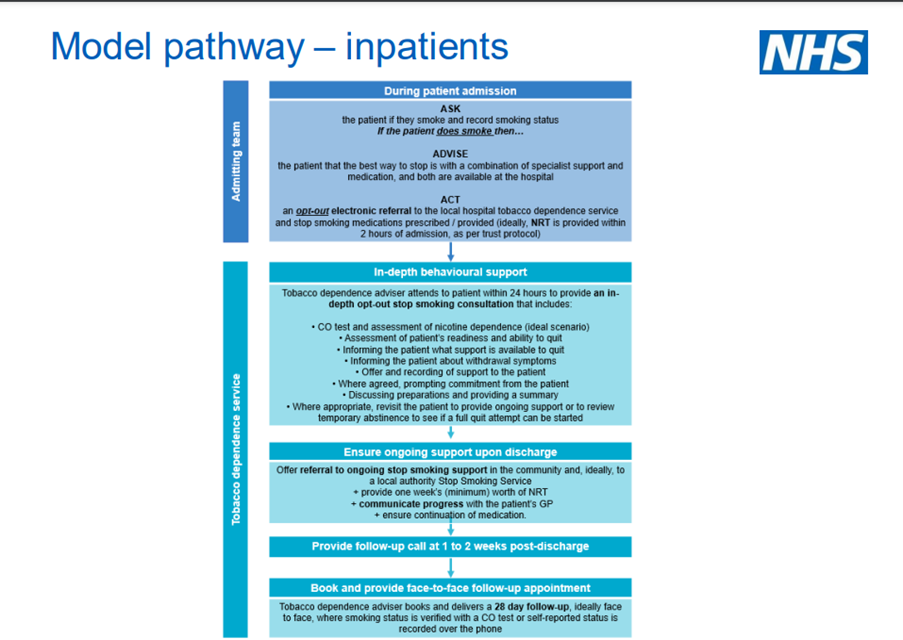
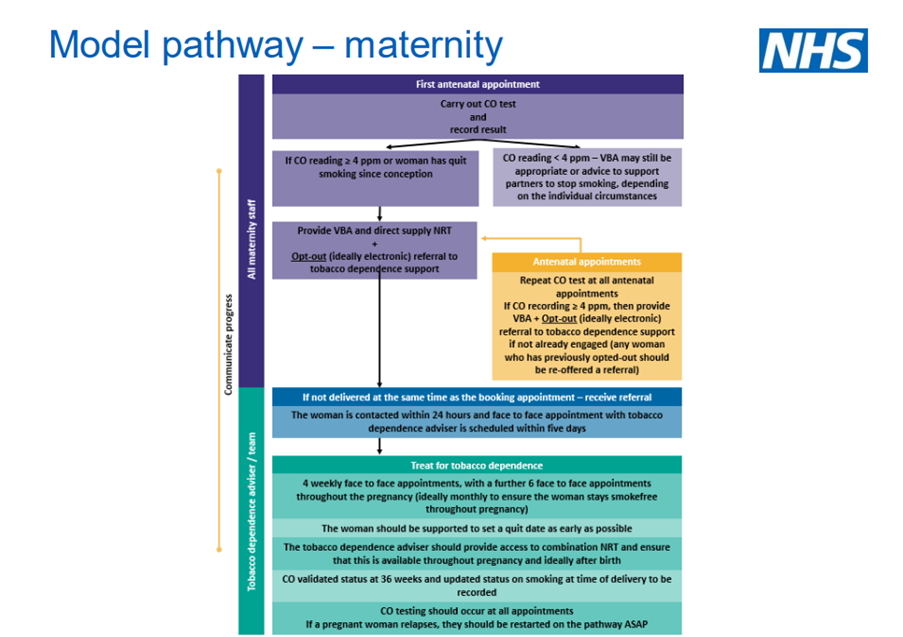
Tobacco dependence treatment services: delivery model - NHS England & NHS Improvement
Recommended Model: Mental Health
The recommended mental health inpatient pathway is currently based on the evidence generated by the acute inpatient model of care. However, adaptations will neeed to be made to ensure that this care model is best suited for mental health services and their users.
Areas where variation is anticipated include:
- Admission: in many cases there may be a pre-agreed plan for smokers who are admitted to mental health settings that can be activated. If not, NRT needs to be started upon admission to tackle nicotine withdrawal, but other elements, including a visit by a tobacco dependence adviser within 24 hours, may need to vary - for example, if a patient is in crisis and isn't able to make an informed decision about starting a quit attempt or if multiple visits are required to build trust.
- Revisit and recheck: mental health admissions tend to have a longer length of stay. We expect up to four additional face-to-face appointments during the admission to ensure that all patients are seen at least weekly for the first month and that time and resource is available to build trust, which will help when having conversations about agreeing to quit or converting temporary abstinence into a full quit.
- Step-down care: a significant level of mental health service is delivered in community settings, and, following discharge, prolonged (in comparison to non-mental health pathways) treatment with pharmacotherapy and behavioural support as per the SCIMITAR+ study (Gilbody, 2019) may be more approporiate to support some mental health patients (recognising that full outpatient/community care will follow in 2022/23 and 2023/24.
The Prevention Programme platform contains models that are in development by other areas and will continue to be updated.
Patients who receive support for tobacco dependence treatment in hospital should be referred to their local community stop smoking service upon discharge, to ensure a continuity of care and ongoing support for their quit journey.
Tobacco prevention is a Hampshire and Isle of Wight system-wide approach, meaning that collaboration between the NHS, our partners in local authority public health and community stop smoking services is essential to help people to quit smoking and improve their health.
If you would like help to stop smoking or other healthy lifestyle advice, you can find your services below:
Find further news and updates from the prevention briefing here.